Hand Osteoarthritis
Arthritis—literally meaning “inflamed joint”—can affect any joint in your body, including those between the 29 bones of the wrist, hand, and fingers. When arthritis occurs in the hand, it can cause pain and limit your ability to perform daily tasks. The most common types of hand arthritis include osteoarthritis, post-traumatic arthritis (following an injury), and rheumatoid arthritis. In osteoarthritis, the smooth cartilage that covers joint surfaces gradually wears away or becomes damaged over time.
Causes
A healthy joint is made up of two smooth, cartilage-covered bone surfaces that move easily against one another. When these smooth surfaces begin to deteriorate, the joint no longer functions properly, leading to arthritis. Additionally, factors such as injury, infection, gout, psoriasis, and other conditions can contribute to the development of arthritis in the hand.
Signs and symptoms
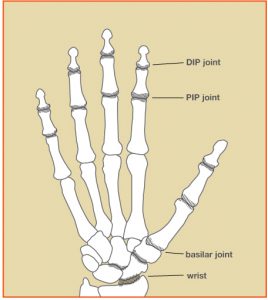
Arthritis in the hand most frequently affects three areas:
- At the base of the thumb where the thumb meets the wrist (the trapeziometacarpal or basilar joint)
- At the joint closest to the fingertip (the distal interphalangeal or DIP joint)
- At the middle joint of a finger (the proximal interphalangeal or PIP joint)
All forms of hand arthritis can result in stiffness, swelling, pain, and joint deformities. Osteoarthritis, in particular, may cause bony enlargements known as Bouchard’s nodes at the middle joint or Heberden’s nodes at the end joint of the finger. Arthritis at the basilar joint of the thumb can lead to noticeable swelling, a bump, and a deep, aching pain. A weakened grip or pinch may make everyday tasks like opening a jar or turning a key difficult.
Treatment
Osteoarthritis diagnosis
Your doctor will begin by asking about your hand and joint health, and how your symptoms affect your daily activities. A physical examination of your hands is performed to observe any changes in appearance or function. X-rays are commonly used to identify signs of osteoarthritis, such as joint space loss or the formation of bone spurs.
Osteoarthritis treatment
The main goals in treating osteoarthritis are to reduce pain and restore function. Short periods of rest—achieved by modifying activities or using a splint—can be beneficial. When rigid splints are too restrictive, soft, supportive sleeves may offer relief. Applying heat through methods such as paraffin baths or warm compresses can soothe the joints and help maintain mobility. It’s essential to keep the fingers as active as possible, and hand therapists can teach joint protection exercises and suggest activity modifications. Anti-inflammatory medications or steroid injections into the joint may alleviate pain, but they do not cure the arthritis.
If non-surgical treatments do not provide sufficient relief, surgery might be considered. Typically, you will decide together with your doctor when surgery is the best option. The aim of surgery is to maximize function and minimize pain. One surgical option is joint fusion, in which damaged cartilage is removed and the bones are joined together. This procedure stops joint movement, thereby eliminating pain. Another option is joint reconstruction, where the damaged joint surface is replaced with either your own soft tissue or an implant. The choice of surgery depends on the specific joints involved, your anatomy, and your lifestyle. Your hand surgeon will help determine the most suitable surgical approach for your situation.
Key Takeaways